Sulmuna R, Raghu Dhanapal, Jaish Lal, Gomakumar
Department of Oral Pathology and Microbiology, Rajas Dental College & Hospital, Kavalkinaru,Thirunelveli, Tamil Nadu
Received : 18-01-2022
Revised : 01-03-2022
Accepted : 15-03-2022
Address for correspondence
Sulmuna R, Post Graduate student, Department of Oral Pathology and Microbiology, Rajas Dental College & Hospital, Kavalkinaru, Thirunelveli, Tamil Nadu. E-mail: sulmuna96@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-Noncommercial ShareAlike 4.0 license, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
How to cite this article: Sulmuna.R, Dhanapal R, Lal J, Gomakumar. Analysis of Keratinization in Post-Menopausal Women and Women of Reproductive Age Using Cytological Smears – A Preliminary Study. J Oral Biomed Sci 2022;1:7-10
Abstract
Alterations in the sex hormones causes significant variation in gingival keratinization. The study is based on comparing the pattern of keratinization in post-menopausal women and women of reproductive age. The aim of this study is to evaluate and compare the pattern of keratinization in post-menopausal women and women of reproductive age using Papanicolaou stain. Sample collection was done. Papanicolaou staining procedure was carried out. Stained slides were viewed under microscope for the evaluation. The results were entered in spss software version 21. Comparing the cell differentiation types between the study groups and Comparison of cell differentiation types within the study groups were done. Alteration in sex hormones cause variation in gingival keratinization. Physiological levels of estrogen and progesterone in pregnancy stimulates prostaglandin synthesis.
Key words: Keratinization, post-menopausal women, cytology
Introduction
Keratinization of gingiva is required for normal gingival health. Hormones have an influence on keratinization of gingiva. Alterations in the sex hormones causes significant variation in gingival keratinization. The present study is at comparing the pattern of keratinization in post-menopausal women and women of reproductive age. The aim of this study is to evaluate and compare the pattern of keratinization in post-menopausal women and women of reproductive age using Papanicolaou stain.
Materials and methods
Comparative study conducted in Department of Oral Pathology & Central research lab, Rajas Dental College and Hospital. Subjects included in study were post-menopausal women above 55 years (n = 10) & women of reproductive age of 18 to 30 years (n=10).
The women with immune compromised state, tobacco related habits, periodontitis, women undergone ovariectomy and other with systemic diseases were excluded from the study.
Results were entered in SPSS software version 21. Frequency of keratinized cells, partially keratinized cells and keratinized cells were evaluated. P value < 0.05 was considered statistically significant
Procedure:
The microscopic slides were cleaned with water, dried and numbered. The subjects were asked to rinse their mouth thoroughly with water. Using a tooth brush the attached gingiva was scraped. Scrapings were smeared on the slide. Slides were fixed in 95% alcohol for 30 minutes. Papanicolaou staining method was used for staining. Standard method of staining was used. Rinse in tap water. Harris hematoxylin 1- 3 minutes, rinse in tap water. Dip the glass slides in 95% ethanol for 10 dips. OG-6(Orange -6) stain for 1.5 minutes, again dip the glass slide in ethanol for 10 dips. Eosin Azure 50(EA50) stain solution-2%W/V for 2.5 minutes. 95% ethanol is used for dipping the glass slides for 2 changes. Glass slides are then placed in ethanol 100% for 1 minute. Clear the glass slides by placing it in xylene for 2 minutes. Mount with DPX mounting medium. Place the cover slip. The slides are examined under microscope.
Parameters to be studied:
Keratinization of the gingiva were seen distinctly from shades of orange to shades of red to pink. Matured keratin stained in shades orange, immature keratin showed pink stain.
Results:
Comparing the cell differentiation types between the study groups
| Category | Type of cells | Mean± SD | t(df) | p value |
| Reproductive women | Pink cells | 81.7±6.68 | 4.8(18) | <0.001* |
| Post menopausal women | 42±25 | |||
| Reproductive women | Orange cells | 18.2±6 | -4.8(18) | <0.001* |
| Post menopausal women | 58±25 |
Comparison of cell differentiation types within the study groups
| Category | Type of cells | Mean± SD | p value |
| Pink cells | Reproductive women | 81.7±6.68 | <0.001* |
| Orange cells | 18.2±6 | ||
| Pink cells | Post menopausal women | 42±25 | 0.342 |
| Orange cells | 58±25 |
Pink cells were found to be high in reproductive women with mean value of 81.7 with p value <0.001 which is statistically significant. Orange cells were found to be high in post-menopausal women with mean value of 58 and p value <0.001 which is also statistically significant.
When comparing within the groups pink cell in reproductive women were found to be higher and statistically significant. But when comparing the pink and orange cells in post-menopausal women it is statistically insignificant with p value 0.342
Discussion:
Alteration in sex hormones cause variation in gingival keratinization. Orangophilic cells are highly keratinized cells and the eosinophilic that are described as low keratinized cells3. In our study, high eosinophilic cells were noted in women of reproductive age. Orangeophilic cells were found to be high in post-menopausal women.
Physiological levels of estrogen and progesterone in pregnancy stimulates prostaglandin synthesis.4 Due to the vascular changes caused by hormones there is more florid response to the irritant effects of dental plaque.5 Estrogen causes changes in the keratinization of the gingival epithelium and alters the degree of polymerisation of ground substance.
Increased edema, erythema, gingival crevicular exudate and hemorrhagic gingival tissues may also be observed due to the effects of estrogen.6 Sex steroid hormones have been shown to have effects on cellular growth, proliferation and differentiation in target tissues including keratinocytes and fibroblasts in the gingiva.7
The effect of estrogen on periodontium on the cellular aspect is that it decreases the keratinization and increases the epithelial glycogen. It also alters the degree of polymerization of ground substances.8 This results in diminution in the effectiveness of the epithelial barrier. Estrogen the sex hormone causes significant alteration in keratinization. Hence it has a significant impact on gingival tissues.
Conclusion:
In our study there was an increase in keratinization in post-menopausal women. Women of reproductive age has a decrease in keratinization. Hence, there is a predisposition to benign reactive lesions in reproductive women.
Conflict of interests : None
Financial support and sponsorship : Nil
References:
- Balan U, Gonsalves N, Jose M, Girish KL. Symptomatic changes of oral mucosa during normal hormonal turnover in healthy young menstruating women. JContemp Dent Pract. 2012 1;13:178-81..
- Anuradha A,SivapathasudharamB. Image analysis of normal exfoliated gingival cells. Indian J Dent Res-2007;18:63-66.
- S. Preethi, B. Sivapathasundharam. Will Papanicolaou stain be the new stain for keratin?. Journal of Histotechnology-2015;26;38:9-13.
- Nirola A, Batra P, Kaur J. Ascendancy of sex hormones on periodontium during reproductive life cycle of women. J Int Clin Dent Res Organ-2018;10:3-11
- SahuM, Suryawanshi H, Nayak S, Kumar P. Cytomorphometric analysis of gingival epithelium and buccal mucosa cells in type 2 diabetes mellitus patients. J Oral Maxillofac Pathol. 2017;21:224-228.
- MascarenhasP, Gapski R, Al-Shammari K, Wang HL. Influence of sex hormones on the periodontium. J Clin Periodontol. 2003 ;30:671-81.
- JaishreeTukaram Kshirsagar, Balamurugan. Role of sex hormones in periodontium during pregnancy: A review. IJADS. 2018;4: 168-173.
- Min Wu, Shao-Wu Chen, Shao-Yun Jiang, Relationship between Gingival Inflammation and Pregnancy.Mediators of Inflammation, 2015;1-11
- Rajkumar NG, Bharath TS, Manjunath K, Saraswathi TR, Ramachandran CR. Cytological changes and pattern of keratinization in palatal mucosa of reverse smokers: A pilot study. Journal of Orofacial Sciences. 2010 ;1;2-7.
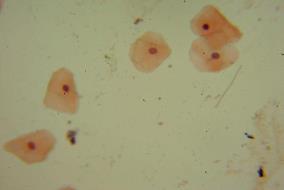
Fig 1:Eosinophilic cells
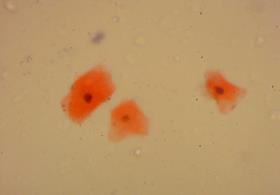
Fig 2: Orangophilic cells

