Lembai Sneha, Mathew Josey, George Liza, Paul Sinju
Department of Conservative Dentistry and Endodontics, Annoor Dental College and Hospital, Muvattupuzha
Running title – Management of blunderbuss canal with periapical cyst
Received: 11-02-2024
Revised: 15-02-2024
Accepted: 22-02-2024
Address for correspondence: Dr Sneha Lembai. PG Student, Department of Conservative Dentistry and Endodontics, Annoor dental college, Perumattom (PO), Muvattupuzha, Kerala-686673, India
Email – snehalembai@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-Noncommercial ShareAlike 4.0 license, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms
How to cite this article: Lembai Sneha, Mathew Josey, George Liza, Paul Sinju. Interdisciplinary management of a maxillary central incisor with blunderbuss canal and large periapical cyst- A Case report. J Oral Biomed Sci 2024; 3(1):41-47
Abstract
Traumatic dental injuries involving dentoalveolar region will affect the teeth and supporting soft and hard tissues. Any traumatic injury during root development will hamper the root end development. Managing an open apex is an arduous task due to complexity of achieving apical seal and the susceptibility of the thin radicular walls to fracture.
This case report depicts, management of a large radicular cyst extending from the periapical region of maxillary anteriors to premolars with root canal treatment of multiple teeth and retrograde MTA apical barrier placement on maxillary central incisor with blunderbuss canal. The blunderbuss canal and compromised crown root ratio of maxillary central incisor necessitated a modified obturation technique and root reinforcement by placing an anatomic Compo Post into the canal, providing structural support and stability. MTA retrograde filling was applied to seal the apex, enhancing the root’s integrity and ensuring the long-term functionality of the maxillary central incisor. This report will guide the clinicians in management of cases with blunderbuss canals.
Key words: radicular cyst, blunderbuss canal, anatomic composite post
INTRODUCTION
Physiological root development and closure takes approximately 3 years following tooth eruption. But during this period if caries exposure or trauma occurs, necrosis of pulp occurs and root development gets hampered.1The resultant immature root will have an open apex. Immature apex causes problems such as thin dentinal walls, frequent periapical lesions, large open apices, short roots, discoloration of teeth and fracture of crown. This makes endodontic treatment more challenging due to thin dentinal walls which are fracture susceptible and difficulty in obtaining apical seal during obturation. A blunderbuss canal is a type of open apex, characterized by an incompletely formed root where the apical canal diameter is larger than coronal diameter.2
Apexification plays a crucial role in managing open apex cases by providing a hard tissue barrier at root end with efficient apical seal, facilitating 3D obturation and preventing future complications. To circumvent the constraints of standard long-term calcium hydroxide apexification processes, single-step apexification using materials, like mineral trioxide aggregate (MTA), has been proposed. Torabinejad et al evaluated MTA as root end filling material and found it to be superior than other materials.3 However, proper compaction of MTA in tooth with wide open apex can be difficult to achieve.
As a result, this case report discusses a new strategy for employing an anatomic composite post after periapical surgery of a large radicular cyst and retrograde MTA filling, that provides sufficient bonding and reinforcement to blunderbuss canal.
CASE REPORT
A 20-year-old male patient came to our department with the chief complaint of pain and pus discharge in relation to the upper left front tooth region since 2 months. The Pain was found to be intermittent in nature, with similar occurrence 1 year before and had a history of trauma following a bike accident 10 years back. On clinical examination, 21 was discolored with Ellis class II fracture and grade I mobility. A sinus opening with pus discharge was located on palatal aspect between 22 and 23. On cold and electric pulp test, 21,22,23,24 &25 did not show any response, suggesting 21,22,23,24 &25 were non-vital. CBCT of maxillary anteriors and premolars showed a large periapical lesion between 21 to 25 of approximate size 23.4 mm x 12.2mm with both buccal and palatal cortical plate perforations. Sinus wall involvement was detected with close proximity to incisive fossa. Radiographic evaluation showed blunderbuss canal with extensive internal and external resorption with compromised crown root ratio was found on 21(Figure1 shows PREOP CBCT). Correlating clinical and radiographic findings, provisional diagnosis was necrotic pulp and periapical cyst on 21,22,23,24 & 25 with blunderbuss canal on 21.
TREATMENT PLAN
The endodontic treatment was planned for teeth 21,22,23,24 & 25. Obturation of 21 was done after retrograde MTA apexification and radicular reinforcement using an anatomic compo-post.
TREATMENT DONE
PRESURGICAL PHASE
Access opening, cleaning and shaping was done on 21,22,23,24& 25 followed by placement of intracanal medicament of Ca (OH)2 {RC Cal (Prime Dental products, Mumbai, India)} for 2 weeks. All other tooth except 21 were obturated using lateral condensation technique (Figure 2 shows obturation using lateral condensation method).
After initiation of RCT, a novel technique was planned for condensation of MTA of 21, since there was no platform available against which MTA can be condensed. A rolled cone was placed in canal leaving apical 4mm for retrograde filling of MTA during surgical phase (Figure 3 shows placement of rolled cone). This was planned to be removed after the completion of surgical phase. Root canal orifice was sealed and surgery was planned.
SURGICAL PHASE
Full thickness flap reflected extending from 21 to 25 and cyst enucleation was done under GA. After controlling haemorrhage, ProRoot MTA was placed into the root-end cavity over the rolled cone of 21 and condensed with a plugger followed by intermittent suturing. Radicular cyst was confirmed by histopathological examination (Figure 4 shows periapical surgery).
RADICULAR REINFORCEMENT TECHNIQUE
Tooth was evaluated after 2 weeks showed complete retraction of sinus tract suggestive of healing. The rolled cone was removed and ensured that MTA barrier was adequate at apical third of root canal. This was confirmed on radiograph. A prefabricated fiber post #3 (Reforpost, Angelus, Londrina, Brazil) was taken & checked for fit inside the canal. The Post was cleaned with alcohol, surface treatment done with H2O2 & a layer of silane (Monobond plus, Ivoclar-Vivadent, Mumbai, India) was applied for 1 minute. Flowable composite added on the post and cured for 30 s and later radiograph was taken to confirm fit of post in the canal. Additional layers of composite (Ivoclar Vivadent Tetric N-Ceram) were added to the post and were cured, and after each addition fit of the post was confirmed by a radiograph. After adequate thickness of the post was achieved, a non-rinse conditioner (ParaBond, Coltene, Altstatten, Switzerland) applied to the canal for 30 seconds, followed by drying the canal for 2 seconds. Using a microbrush, ParaBond Adhesives A and B (Coltene, Altstatten, Switzerland) applied into the canal for 30 seconds. ParaCore cement (Coltene, Altstatten, Switzerland) was then introduced into the canal and the post was carefully inserted to its full depth, light-cured for 40 seconds (Figure 5 shows radicular reinforcement technique).
Follow-up radiographs after 3month,6 month (Figure 6A & 6B) and Post treatment CBCT after 1 year (Figure 7) demonstrated a significant reduction of periapical radiolucency, with no symptoms.
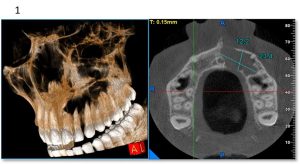
Figure 1– Pre op CBCT
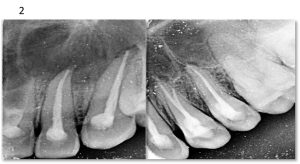
Figure 2- obturation using lateral condensation method
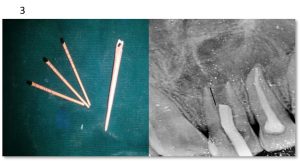
Figure 3 – Roll cone placement

Figure 4 – Periapical surgery

Figure 5 – Post and Core
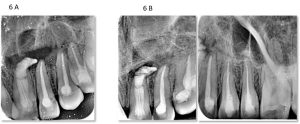
Figure 6A, 6B – 3 and 6 month follow up radiograph

Figure 7 – 1 year follow up cbct
DISCUSSION
Management of a tooth with blunderbuss canal with thin fragile root dentin, with a large radicular cyst was quite challenging and thus a novel approach was needed compared to normal root canal treatment. Regenerative endodontics cannot be employed in this case as regenerative potential of stem cells and signaling molecules locally available in the periapical region of teeth were scarce due to longstanding radicular cyst.
Orthograde apexification cannot be done as there was lack of control in achieving apical seal due to large apical diameter of blunderbuss canal. In this case, considering the extension of radicular cyst and limitation of orthograde apexification, periapical surgery under GA with retrograde apexification using MTA was opted.
Due to the presence of calcium and phosphorus ion, a hard tissue barrier is formed by MTA. It is biocompatible to periodontal tissues due to formation of hydroxyapatite & cellular cementum deposition adjacent to MTA filling, which results in regeneration of periradicular tissues in a short duration.4 In this case, Ca (OH)2 medicament was placed for 2 weeks before the final obturation with MTA to reduce the bacterial infection caused by necrotic pulp.5 A rolled cone was placed leaving a space of 4 mm of apical third for retrograde filling of MTA during periapical surgery. This was temporarily placed to create a platform to condense MTA from root apex and was later removed.
A fiber post was chosen as the obturating material because it bonds well with composite, reinforces the root, and has a similar elastic modulus to that of dentin, thus reducing the risk of crack propagation & fracture.6
Inserting a conventional fiber post into a blunderbuss canal, often shows a loosely fitting post with wide space all around the post inside the canal with no retention. Additionally, a very thick layer of cement is required to fill the space between canal walls & loosely fitting post. This increases the risk of adhesive failure and post debonding. Therefore, an anatomic custom post which is similar to canal shape with thin layer of adhesive cement was the suitable solution for retention. A similar case of MTA apexification and subsequent reinforcement with anatomic compopost showed reduced periapical radiolucency in the 1st 6 months followed by complete healing after 24 months.7
A dual cured, glass reinforced composite (Paracore), provided predictable polymerization even with lack of access to light. In this case, periapical extrusion of MTA observed in CBCT is not expected to affect periapical healing and cause further complications. Demiriz et al presented a similar case with severe iatrogenic MTA extrusion. Without any further intervention, lesion completely healed and this may be because of beneficial effects of MTA like biocompatibility, regeneration of periapical tissues & deposition of bone.8 Moreover, MTA prevents continued periapical tissue irritation owing to its superior sealing capabilities, thus promoting an ideal environment for periapical healing.8
CONCLUSION
Effective management of large radicular cysts with blunderbuss canals often requires an interdisciplinary approach between Endodontists and Maxillofacial surgeons. Retrograde root end filling of MTA by surgical intervention provided faster healing of lesion. Radicular reinforcement successfully achieved by using custom-made compo post. follow up visits and routine radiographic examinations are equally important.
REFERENCES
- Salgar AR, Chandak MG, Manwar NU. Blunder buss canal: A challenge for endodontist. Endodontology. 2011: 1;23:77-81.
- American Association of Endodontists, Glossary of endodontic terms.8th Edn, Chicago 2012.
- Torabinejad M, Watson TF, Pitt Ford TR. Sealing ability of a mineral trioxide aggregate when used as a root end filling material. J Endod. 1993 ;19.
- Torabinejad M, Abu-Tahun I. Management of teeth with necrotic pulp and open apices. Endod Topics. 2012; 23:105–30.
- Afonso T, Sá de Andrade Moura Pega ML, da Costa Michelotto AL, Coelho Abrantes AM, Oliveiros B, Palmeirão Carrilho EV, et al. Effect of calcium hydroxide as intracanal medication on the apical sealing ability of mineral trioxide aggregate (MTA): An in vitro apexification model. J Health Sci Inst. 2012;30:318–22.
- Manhart J. Fibre reinforced composite endodontics post. Endod Prac.2009;16:6-20.
- Pratima M, Abraham D, Singh A, Ahuja R, Kumar A. Management of Blunderbuss Canal with a Single Visit Post-Core Buildup: A case report. Inter J Med Scie.2017;4.
- Demiriz L, Bodrumlu EH. Severe unintentional extrusion of mineral trioxide aggregate during apexification. Indian J Dent Res. 2017;28:341-343.
Conflict of interest: None
Source of support: Nil

