Peter Joji, Sreenivas Rajeswari, Thomas Priya, Mathew Deepu George
1Department of Oral & Maxillofacial Surgery, Annoor Dental College and Hospital, Muvattupuzha
2Department of Oral & Maxillofacial Surgery, Annoor Dental College and Hospital, Muvattupuzha.
Running title – Traumatic bone cyst
Received: 11-06-2023
Revised: 15-06-2023
Accepted: 22-06-2023
Address for correspondence: Dr. Rajeswaari Sreenivas, Post Graduate, Department of Oral and Maxillofacial Pathology & Microbiology, Annoor Dental College & Hospital, Muvattupuzha, Kerala, India
Email – rajusreenivas22@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-Noncommercial ShareAlike 4.0 license, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms
How to cite this article: Peter J1, Sreenivas R2, Thomas P2, Mathew D G. Traumatic bone cyst presenting as an asymptomatic radiolucent mandibular lesion- A case report. J Oral Biomed Sci 2023; 2(2):82-86
Abstract
A traumatic bone cyst (TBC) is an asymptomatic, uncommon non-neoplastic lesion of the jaws that is considered as a “pseudocyst” because of the absence of an epithelial lining. It is diagnosed during routine dental radiographic examination. Here we present a case report of a 14‑year‑old female patient with an accidental finding of a radiolucency in the periapical region of 45,46 & 47 on the routine radiograph. The differential diagnosis was considered to be radicular cyst, Stafney’s bone defect/ cyst, aneurysmal bone cyst. The aim of the present paper is to describe the clinical, radiographic and histologic findings of traumatic bone cysts
Key words: Traumatic bone cyst, Pseudocyst, Mandible, Interdental scalloping
Introduction
Traumatic bone cysts(TBCs) are fluid-filled or empty intra-osseous lesions found most commonly in the proximal metaphyseal region of the long bones in children and adolescents1. It was first described in 1929 as a distinct entity2. In the jaw bones they are usually seen in the mandible (89%). Only a few cases have been reported in the condylar and anterior regions of the mandible3,4. The maxilla was involved in 11% of the cases 4. This lesion lacks an epithelial lining, so it represents a pseudocyst rather than a true cyst5. TBCs are considerd by the World Health Organisation under the category of bony lesions with other lesions such aneurysmal bone cysts, fibrous dysplasia, ossifying fibromas, central giant cell granulomas, and cherubism 6. The diagnostic criteria of TBC were established in1946. The criteria for diagnosing a cystic lesion as solitary bone cyst is that it should be a single lesion without an epithelial lining, surrounded by bony walls and either lacking contents or containing liquid and/or connective tissue7. The solitary bone cyst occurs in young individuals. It mostly seen in the second decade of life; the approximate mean age of patients is 20 years6 and shows a male predilection8
Here we present a unique case of traumatic bone cyst which was clinically diagnosed as a radicular cyst because of its association with caries teeth.
Case report
A 14-year-old female patient reported to a private dental clinic with a chief complaint of decayed lower right back tooth region of 6-month duration. The patient was completely free of symptoms. There was no expansion of cortical bone, either buccally or lingually. No palpable lymph nodes were present. There was secondary dentinal caries in relation to 46 & 47, but the associated tooth were vital. Patient gave a history of fall 8 months back leading to trauma to the right side of the face. A routine radiographic examination showed an extensive, unilocular, well-defined radiolucent lesion, with well-corticated margins noted extending from periapical area of 44, up to mesial root of 47 regions. No root resorption in relation to 44,45,46& 47 was noted. There was thinning of buccal & lingual cortex. Cystic lesion was seen as a domelike projection that scallops upward between the roots of 45 46 & furcation area of 46 (Figure 1).
Based on the clinical and radiographic features the clinician gave a provisional diagnosis as radicular cyst and differential diagnosis as odontogenic keratocyst. Later an enucleation was done and bleeding was induced into the lesion. Then the specimen was sent for histopathologic examination. 4 bits of formalin fixed brown coloured, firm soft tissue specimens of size 10x5mm were received in the lab and sent for processing (figure 2)
On microscopic examination, a fibro-myxomatous connective tissue exhibiting spindle and plump shaped fibroblasts and capillary vessels were seen. Section also showed mild chronic inflammatory cell infiltrate, spicules of vital bone and extravasated RBC’s (figure 3) Correlating the clinical, radiographic, histopathologic features a diagnosis of traumatic bone cyst was made.
Postoperative recovery was uneventful. With a 2-month follow-up period, the clinical examination showed resolution of the lesion and radiographic examination showed evidence of new bone formation (figure 4)
Discussion
The case presented clinically as an asymptomatic radiolucency associated with caries 46,47. The differential diagnosis considered based on the clinical features were radicular cyst, Stafney’s bone defect/ cyst, aneurysmal bone cyst and traumatic bone cyst.
Radicular cyst is a common inflammatory odontogenic cyst associated with non-vital or caries tooth. Since the tooth associated with the lesion had caries, radicular cyst was considered as the first differential diagnosis. Histologically radicular cyst is lined by non-keratinized stratified squamous epithelium of varying thickness, may show arcading pattern with intense inflammatory infiltrate5. But in our case the lining epithelium was absent and only a thin fibrous connective tissue was present.
Another differential diagnosis considered was Stafne bone cyst. These are asymptomatic bone lesions located lingually on the posterior mandible below the inferior alveolar canal which occurs as developmental defect containing a portion of submandibular salivary gland which when examined histologically will show normal submandibular gland tissue5. Since our case did not show such features this entity was also ruled out.
Aneurysmal bone cyst was also considered as another differential diagnosis. It is a benign cystic bone lesion, composed of blood-filled spaces that are separated by connective tissue septa containing fibroblasts, osteoclast-type giant cells and reactive woven bone5. None of these features were seen in our case.
Traumatic bone cyst was also considered as another differential diagnosis. It is an asymptomatic, slow-growing, unusual, non – neoplastic, pseudocystic cavity in the bone. Radiographically it is seen as a well-defined, unilocular, radiolucent lesion with a festooned, scalloping seen between the roots of tooth. It is seen above the inferior alveolar nerve canal 5. On surgical exploration the cystic cavity will be empty. Histopathologically, there is no evidence of lining epithelium, only fibro collagenous connective tissue is present. We saw similar findings in our case. So based on the clinical, radiographic & histopathologic features, a final diagnosis of traumatic bone cyst was made.
The traumatic bone cyst is a rare entity that was initially reported by Lucas and Blum in 1926 and subsequently in 1946 by Rushton as a solitary cyst without epithelium 9. Traumatic bone cysts may be classified as unicameral, simple, solitary, hemorrhagic, or idiopathic10 The pathophysiology of solitary bone cyst is unknown; however, several theories have been proposed9 The most popular theory on the origin of traumatic bone cyst is Trauma haemorrhage theory (figure 5). Intramedullary haemorrhage due to trauma and the liquefaction necrosis of the subsequently formed blood clot leads to pseudocyst formation. The later expansion of the cystic lesion can be due to the enzymatic activity which destroys the surrounding bone10
Majority of solitary bone cysts contain only air or some other gas. Some contain blood or serosanguineous fluid, support the concept of a haematoma breaking down. The breakdown products of haemolysis produce a local rise in osmotic pressure 1. Toller (1964) has demonstrated that the osmotic tension of traumatic bone cyst fluid was higher than that of the patient’s blood. This can also be a reason for cyst expansion1
These lesions are frequently found accidentally during routine radiological examination since they are not associated with any symptoms. Approximately 10%-30% of the cases have symptoms like pain 5,7. Tooth sensitivity, paresthesia, fistulas, delayed permanent tooth eruption, inferior alveolar canal displacement, and pathologic fracture of the jaw are some of the less frequent symptoms 11,12
Radiographic features are similar to that of other odontogenic and nonodontogenic radiolucent jaw lesions .TBC usually seen as a radiolucent, unilocular, well-defined, isolated lesion with irregular or scalloped borders that extended to the interdental bone spaces. It have a festooned, scalloped, or lobular pattern13. A “scalloping effect” is seen when a traumatic bone cyst exist between the tooth’s roots. The multilocularity is caused by sloping of the endosteal surface of the buccal or lingual cortical plate11,14
Histopathology of traumatic bone cyst consists of a loose vascular fibrous tissue membrane of variable thickness with no epithelial lining. Fragments of fibrin with enmeshed red cells may be seen. Haemorrhage, hemosiderin pigment and scattered small multinucleate cells are often found. In long standing cases some cyst walls appear more densely fibrous. The adjacent bone shows osteoclastic resorption on its inner surface1
The final diagnosis of a traumatic bone cyst is made after the histopathological examination. The material available for histology is usually sparse because of the difficulty in removing the thin connective tissue membrane. Surgeons often face an empty cavity, however there may be blood, serum, or both15. Surgery or curettage of the bone walls is the preferred therapy for traumatic bone cysts, which usually results in short-term recovery. Recurrences are uncommon and generally occur three months after surgery 15
Conclusion
Trauma may have a significant role in the development of TBCs, although the evidence for its etiopathogenesis is yet insufficient. Therefore, it is crucial to correlate the given history, clinical findings, and radiographic examination and histopathologic findings in order to make a confirming diagnosis and then perform the necessary treatment procedures.
Conflict of interest: None
Source of support: Nil
References
- Shear M, Speight PM. Cysts of the oral and maxillofacial regions. John Wiley & Sons; 2008 Apr 15. 4th edition.
- Lucas CD, Blum T. Do all cysts in the jaws originate from the dental system. J Am Dent Assoc. 1929;16:647–61.
- Kumar LS, Kurien N, Thaha KA. Traumatic bone cyst of mandible. J Maxillofac Oral Surg. 2015;14(2):466–9.
- Satish K, Padmashree S, Rema J. Traumatic bone cyst of idiopathic origin? A report of two cases. Ethiopian journal of health sciences. 2014 Apr 14;24(2):183-7.
- Neville, B.W., Damm, D.D., Allen, C.M. and Chi, A.C. (2016) Oral & Maxillofacial Pathology. 4th Edition, WB Saunders, Elsevier, Missouri, 604-605.
- Donkor P, Punnia-Moorthy A. Biochemical analysis of simple bone cyst fluid—report of a case. Int J Oral Maxillofac Surg. 1994;23(5):296–7.
- Rushton MA. Solitary bone cysts in the mandible. Br Dent J. 1946;81:37–49.
- Ahmed K, Al-Ashgar F. Maxillary solitary cyst: review of literature and case report. Saudi Dent J. 1991;3(3):109–13.
- Karthik KP , Balamurugan R and SahanaPushpa T. Traumatic bone cyst of anterior mandible: A surgical approach. Dent Oral Maxillofac Res, 2019. Volume 5: 1-4.
- Martins-Filho PR, Santos TD, Araújo VL, Santos JS, Andrade ES, Silva LC. Traumatic bone cyst of the mandible: a review of 26 cases. Brazilian journal of otorhinolaryngology. 2012;78:16-21.
- Thelekkat Y, Basheer SA. Traumatic bone cyst in the mandibular ramus–A diagnostic dilemma. Nigerian Journal of Clinical Practice. 2022 Aug 16;25(8):1382-5.
- Dhopte A, Tandon P, Shenoy M, Mustilwar R, Abdul NS, Bagde H, Singh R, MUSTILWAR R. Traumatic Bone Cyst of the Anterior Mandibular Region: A Case Report. Cureus. 2022 Nov 10;14(11).
- Whinery JG: Progressive bone cavities of the mandible: a review of the so-called traumatic bone cyst and a report of three cases. Oral Surg Oral Med Oral Pathol. 1955, 8:903-16. 10.1016/0030-4220(55)90289-9.
- Suei Y, Taguchi A, Tanimoto K. A comparative study of simple bone cysts of the jaw and extracranial bones. Dentomaxillofac Radiol. 2007;36(3):125–9.
- Pindborg JJ, Kramer IR, Torloni H: Histological typing of odontogenic tumours, jaw cysts, and allied lesions . World Health Organization, Geneva, Switzerland; 1971. 44 (67).
Figures
Figure 1 (a) CBCT image showing the radiolucent lesion in the body of the mandible. 1(b) The CBCT shows a well‑defined, unilocular osteolytic hypodense lesion with scalloped borders between roots of 45 & 46
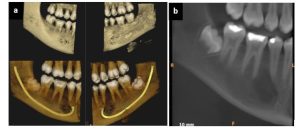
Fig 2 – Gross specimen with 4 bits soft tissue

Figure 3 – Low power view of traumatic bone cyst showing spicules of vital bone (black arrow), areas of thin fibrin layer (red arrow) and extravasated RBC’s (yellow arrow)
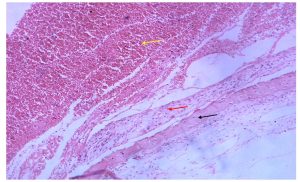
Figure 4 – Post operative radiograph showing new bone formation

Figure 5 – Flow chart on the trauma – haemorrhage theory of traumatic bone cyst origin


