OBTURATION OF PRIMARY MANDIBULAR SECOND MOLAR WITHOUT PERMANENT SUCCESSOR USING BIODENTINETM: A CASE REPORT
Thankachan Saranya P, Peter Joby, Jose Bijimol, Methippara John Joseph, Sebastian Ronin
Department of Pediatric and Preventive Dentistry, Annoor Dental College & Hospital, Muvattupuzha
Received: 18 – 05 – 2022
Revised: 25 – 05 – 2022
Accepted: 24 – 06 – 2022
Address for correspondence: Dr. Saranya P Thankachan, PG Student, Dept. Of Pediatric and preventive dentistry, Annoor dental college, Email id: saranyapthankachan52@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-Noncommercial ShareAlike 4.0 license, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms
How to cite this article: Thankachan S P, Peter J, Jose B, Methippara J J, Sebastian R. Obturation of Primary Mandibular Second Molar without Permanent Successor Using BiodentineTM: A Case Report. J Oral Biomed Sci 2022; 1:84-8
Abstract
The success of pulpectomy treatment depends on removal of infected pulp and filling it with a biocompatible material. In order to achieve it, the clinicians should understand the morphology of the individual root canal and atypical root canal configuration. The purpose of this article was to describe a case of primary mandibular second molar with missing successor tooth. BiodentineTM a new dentine substitute was used as an obturating material for retained maxillary second molar. After 24 months follow up, the success of BiodentineTM for management of primary tooth with chronic pulpitis and missing successor was evaluated and reported.
Keywords: Dentin substitute, BiodentineTM, missing teeth, Pulpectomy
Case report
Congenitally missing teeth (CMT), congenital absence of teeth, congenital dental aplasia, dental agenesis or as usually called hypodontia is one of the most common dental anomaly.Patients with missing teeth may suffer from malocclusion, periodontal damage, insufficient alveolar bone growth, reduced chewing ability, inarticulate pronunciation, changes in skeletal relationships and an unfavorable appearance and other problems,most of which need rather costly and challenging multidisciplinary treatments.
In the primary dentition, the CMT is not frequent, being between 0.1% and 2.4%. However, primary dental aplasia is usually followed by permanent tooth missing. The prevalence of CMT in the permanent dentition excluding the third molars ranges between 0.15% and 16.2%. Japanese people showed the highest rates both in deciduous and permanent dentitions. Indians have shown very small prevalence rates, as two out of three studies in India had rates less than 1% and the other one had about 4% prevalence.[1]
A 9-year-old boy reported in our Department of Paediatric and Preventive Dentistry with a chief complaint of pain on lower right back tooth region. [Fig-1]. History says Patient noticed decayed tooth in lower right back tooth region 4 months, had undergone filling from outside clinic. He experienced pain 3weeks before which was sudden and spontaneous onset, aggravated on having food and night pain also reported. Pain relieved on medication.
During clinical examination it was tender on percussion and palpation. The patient had no significant medical history. Intraoral periapical radiograph of right mandibular region revealed radiolucency involving pulp and furcation area of lower right mandibular second molar teeth with Congenitally missing succedenous tooth beneath to it [Fig-2]. A panoramic radiograph was taken to investigate the absence of any other permanent tooth bud [Fig-3].
Based on the clinical and radiographic examination, acute irreversible pulpitis in relation to right primary mandibular second molar and congenitally missing premolar was diagnosed. Following parental consent, the tooth was anaesthetized with 2% lignocaine hydrochloride 1:2,00,000 epinephrine (Lignox Indoco Remedies Ltd. Mumbai, India) and isolated using a rubber dam.
Access cavity preparation was completed; three canal orifices (mesiobuccal, mesiolingual and distal) were located [Fig-4]. The working length was determined radiographically measuring 16 mm for the distal canal and 16 mm for the mesiobuccal canal and mesiolingual canal [Fig-5].
The root canals were enlarged till 35 K-file (Mani, Inc, Tochigi, Japan). During instrumentation the canals were irrigated using 3% sodium hypochlorite solution and the final irrigation was done with saline. The canals were obturated with Biodentine™ [Fig-6]. Using a measured endodontic plugger the material was vertically condensed from the apex to the canal orifice in both distal and mesiobucal canals . The coronal seal of the endodontically treated tooth was done with glass ionomer cement (GC Fuji II, Tokyo, Japan)[ [Fig-7]. Finally size five stainless steel crown (3M ESPE, St Paul, MN, USA) was cemented using Type 1 glass ionomer cement [Fig-8]. At six and 24 months follow up [Fig-9,10] the tooth revealed no periapical lesion and no evidence of mobility.
Discussion
Maintenance of the retained primary tooth with congenital absence of permanent successor is a challenge to the dentist. This case report describes a retained primary mandibular second molar with missing premolars.
The occurrence of a congenitally missing first permanent molar is a rare finding and the common congenitally missing permanent teeth in the order of frequency are Third molars, second premolars, and lateral incisors. Congenitally missing teeth are common in patients with cleft lip and palate, ectodermal dysplasia, Down syndrome, and so forth, however, it is a rare finding in a non-syndromic healthy patient without the absence of the other teeth[1]
Retained primary teeth having intact crown and root structure with missing successor should be preserved. This would prevent arch length discrepancy and maintain the space without requirement for orthodontic or prosthetic treatment [2].Usually the Obturating material used for filling the root canal space of primary teeth should resorb at a similar rate as the primary root. Various root canal filling materials are available for primary teeth namely, Zinc Oxide Eugenol (ZOE) paste, calcium hydroxide alone or a combination of calcium hydroxide and iodoform paste [3]. ZOE was used as a common material for obturating primary teeth. Accidental extrusion beyond the apex of ZOE remains in the alveolar bone for months to years. The extruded material may also cause a foreign body reaction [4]. Due to this limitation calcium hydroxide based obturating materials were introduced. Calcium hydroxide with iodoform is widely used for obturation of primary teeth due to its better properties compared to ZOE [5]. Primary tooth without permanent tooth bud shows no signs of root resorption. Obturating material for retained primary teeth with missing permanent teeth should be biocompatible and non-resorbable. Guttapercha, Mineral Trioxide Aggregate (MTA) and BiodentineTM should be considered as a root canal filling material for retained primary teeth with missing successor[6]These materials are considered to be biocompatible and non resorbabale.
O’ Sulliavan SM et al., reported a case of 20-year-old male with retained primary mandibular second molar and it was obturated with MTA [7]. Bolla N et al., reported a case of 26-year-old female with retained primary mandibular second molar, obturated with guttapercha [8].
Ganesh Jeevanandan et al reported an unusual case of a primary maxillary second molar with double roots with missing permanent first and second premolars.After 24 months follow up, the success of BiodentineTM for management of primary tooth with missing successor was evaluated and reported[9].
BiodentineTM is considered to be an alternative to conventional calcium hydroxide-based material. It is bioactive calcium silicate-based cement having similar mechanical properties like dentin. The material is available as liquid and powder component. The powder in the capsule contains tricalcium, dicalicum silicate and calcium carbonate. Zirconium dioxide acts as a contrast medium. The liquid component contains an aqueous solution of calcium chloride with an admix of polycarboxylate. The liquid is added to the powder in the capsule and mixed using amalgamator for 30 seconds. The consistency of the material once mixed is similar to zinc phosphate cement. On follow up, the retained primary second molar was normal in function with no associated pain and periapical changes. BiodentineTM has shown to be a biocompatible material having superior sealing properties [10]. It shows deposition of apatitic structures which might increase the marginal sealing of the material.[11] Girish Umashetty et al 2022 in their case report concluded that Success in management of a case of internal resorption depends on early detection, appropriate treatment planning, removal of inflammatory pulp tissue, reinforcement of weaker tooth structure, and a three-dimensional obturation.[12] Pulpal pathology and periapical healing has allowed for the use of bioactive materials, such as Bio-dentine, for more conservative treatment options, thereby avoiding extensive and invasive procedures in preserving the tooth and dentition.
In dentition having retained primary teeth with missing successor BiodentineTM, can be considered as the material of choice for root canal filling. Documentation of such cases is very important for the clinicians with proper follow up clinically and radiographically for successful endodontic treatment. Long term follows up of such cases are required to assess the use of new materials in challenging clinical situation.
Conclusion
This case report presents a primary mandibular second molar with missing premolar. This paper also adds on the use of a new dentin substitute BiodentineTM as a permanent obturating material for such cases with 1 year follow up. Routine radiographic examination is mandatory for patients in whom certain teeth do not erupt at their scheduled time.It is important to recognize the anomaly as early as possible, to guide the occlusion, and to implement multidisciplinary management.
Conflict of interest: None
Financial support and sponsorship: Nil
References
- Rakhshan, “Congenitally missing teeth (hypodontia): a review of the literature concerning the etiology, prevalence, risk factors, patterns and treatment,” Dental Research Journal, vol. 12, no. 1, pp. 1–13, 2015.
- Kokich VG, Kokich VO. Congenitally missing mandibular second premolars. Clinical options. Am J Orthod Dentofacial Orthop. 2006;130:437-44.
- Pinkham JR. Pediatric dentistry: Infancy Through Adolescence. 3rd ed. Philadelphia: W.B. Saunders; 1999:350
- Mortazani M, Mesbahi M. Comparision of zinc oxide and eugenol and vitapex for root canal treatment of necrotic primary teeth. Int J of Paed Dent. 2004;14:417- 24.
- Nurko C, Ranly DM, Garcia-Godoy F, Lakshanya KN. Resorption of a calcium hydroxide, iodoform paste (vitapex) in root canal therapy for primary teeth: A case report. Pediatr Dent. 2000;22:517-19.
- Kubota K, Golden BE, Penugonda B. Root canal filling materials for primary teeth: A review of the literature. Journal of Dentistry for Children. 1992;58:225- 27.
- O’Sullivan SM, Haretwell GR. Obturation of a retained primary mandibular second molar using mineral trioxide aggregate: A case report. J Endod. 2001;27:703- 05.
- Bolla N, Naik BD, Kavuri SR, Velagala LD. Obturation of a retained primary mandibular second molar with missing successor using guttapercha: A case report. JIDA. 2011;5:194-95.
- Jeevanandan G. Obturation of a retained primary maxillary second molar using biodentineTM: a case report. Journal of clinical and diagnostic research: JCDR. 2017 Jan;11(1):ZD34.
- Wang X, Sun H, Chang J. Characterization of Ca3 SiO5 /CaCl2 composite cement for dental application. Dent Material. 2008;24:74-82
- Priyalakshmi and M. Ranjan, “Review on biodentine—a bioactive dentin substitute,” IOSR Journal of Dental and Medical Sciences, vol. 13, no. 1, pp. 13–17, 2014. [13] K. A. DuLac, C. J. Nielsen, T. J. Tomazi
- Umashetty G, Hoshing U, Patil S, Ajgaonkar N. Management of inflammatory internal root resorption with Biodentine and thermoplasticised Gutta-Percha. Case reports in dentistry. 2015 Oct 22;2015.

Fig-1: Clinical picture showing secondary caries in primary mandibular second molar with GIC Restoration
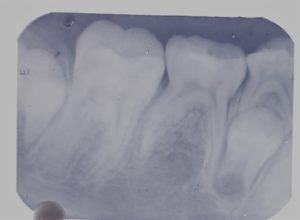
Fig-2: Radiograph showing radiolucency involving pulp in primary mandibular second molar with missing successor
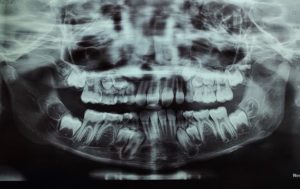
Fig-3:Orthopantomogram showing radiolucency involving pulp in primary mandibular second molar with missing successors.

Fig-4:Intraoral picture showing mesio buccal,mesiolingual and distal canal orifice
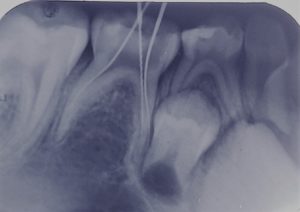
Fig-5:Working length determination

Fig-6: BiodentineTM-powder in capsule and liquid in a pipette

Fig-7: Radiograph showing teeth obturated with Biodentine followed by GIC Restoration

Fig-8: Clinical picture showing teeth restored with stainless steel crown

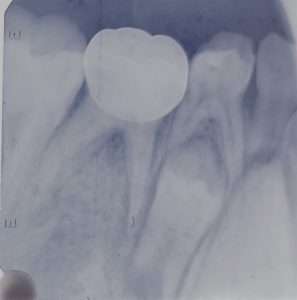
Fig-9,10: Postoperative radiograph showing obturation of primary mandibularsecond molar with BiodentineTM Follow up radiograph after six and 12 months.

