TREATMENT OF A SKELETAL CLASS III CASE WITH CONVENTIONAL ORTHOGNATHIC SURGICAL APPROACH
Sebastian Irin1, Gopikrishnan S1, George Pradeep Philip1, Eldhose K G2
1-Department of Orthodontics and Dentofacial Orthopaedics, Annoor Dental College & Hospital, Muvattupuzha
2- Department of Oral and Maxillofacial Surgery, Annoor Dental College & Hospital, Muvattupuzha
Received: 9 – 05 – 2022
Revised: 23 – 05 – 2022
Accepted: 16 – 06 – 2022
Address for correspondence: Dr. Irin Sebastian, PG Student, Department of Orthodontics and dentofacial Orthopaedics, Annoor Dental College and Hospital, Puthuppady PO, Perumattom, Muvattupuzha. Email Id: irin.sebastian@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-Noncommercial ShareAlike 4.0 license, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms
How to cite this article: Sebastian I, Gopikrishnan S, George P P, Eldhose K G. Treatment of a skeletal class III case with conventional orthognathic surgical approach. J Oral Biomed Sci 2022; 1: 89-96
Abstract
In skeletal Class III cases, it may be difficult to obtain an excellent occlusal outcome only with orthodontic treatment and to maintain a stable post treatment occlusion. There are three main treatment options for correction of skeletal Class III malocclusion: growth modification, dentoalveolar compensation and orthognathic surgery. In most cases, surgical treatment of Class III malocclusion includes mandibular setback, maxillary advancement or a combination of both.
The following is a case report of an ongoing treatment of Skeletal Class III malocclusion due to a prognathic mandible in a 17 year old female patient. The treatment objective was to achieve a more esthetically harmonious facial profile by correcting the skeletal Class III jaw base. The treatment plan included correction of prognathic mandible by surgical line of treatment with conventional orthognathic approach (Bilateral sagittal split osteotomy).
Keywords: Skeletal class III, Orthognathic surgery, Bilateral sagittal split osteotomy
Introduction
Severe dental and facial deformities in adults usually require treatment combined with orthodontics and orthognathic surgery to achieve optimal, stable, esthetic and functional results. Pure mandibular skeletal protrusion, pure maxillary skeletal retrusion, combination of maxillary skeletal retrusion and mandibular skeletal protrusion are the three most common factors contributing to skeletal Class III malocclusion. Pure mandibular skeletal protrusion is commonly cited as the principal anomaly in adult Class III malocclusion.1
A principal component of orthognathic surgery is the bilateral sagittal split osteotomy (BSSO), which is the most commonly performed jaw surgery. It can be performed either with or without upper jaw surgery according to the treatment requirements. Indications for a bilateral sagittal split osteotomy include horizontal mandibular excess, deficiency and/or asymmetry. It is the most commonly performed procedure for mandibular advancement and can also be utilized for a mandibular setback of small to moderate magnitude.2
Diagnosis
A 17 years 6 months old female patient reported to the department with the chief complaint of forwardly placed lower jaw. No relevant pre- and post-natal history or family history was reported. On extraoral examination, the patient showed a concave profile with anterior divergence with potentially competent lips showing 100% incisor exposure on smile with 2 mm of gingival display. Patient had acute nasolabial angle and protrusive lower lip. (Fig: 1)
Intraoral examination showed the patient had mutilated malocclusion with Class III Canine relation, Class III incisor relation with proclined upper anteriors, cross bite irt 11,12,13,21,31,32,41,42,43,44 with mesiolingually rotated 13,15,23,33,35,45,47, spacing between 43 and 44 with missing 16,36,46. (Fig:2)
In OPG, full set of teeth were present except 16, 36 and 46 which were extracted as they were grossly decayed. (Fig: 3) Pre-treatment cephalogram showed CVMI stage 6 indicating completion stage. (Fig: 4)
Cephalometric analysis indicated Class III jaw base due to prognathic mandible with vertical growth pattern. Patient showed increased mandibular plane angle and had proclined upper incisors and retroclined lower incisors. Patient had protrusive lower lip and retrusive upper lip. It was confirmed through cephalometric analysis, that patient had acute nasolabial angle.
Etiology
Patient has prognathic mandible without any immediate familial history.
Treatment Objectives
The treatment objectives were:
- To improve the skeletal jaw relationship by mandibular setback in relation to the cranium.
- To achieve well aligned maxillary and mandibular arches.
- To achieve positive overjet.
- To correct proclined upper incisors, retroclined lower anteriors and anterior crossbite.
Treatment Plan
To correct the skeletal Class III jawbase due to prognathic mandible, it was decided to go ahead with conventional orthognathic surgery approach. The treatment procedure started with extraction of lower third molars on both sides. In presurgical orthodontics, levelling and alignment of dental arches were done and all dental decompensations were removed to maximize optimal surgical repositioning of the jaw. (Fig: 6)
After presurgical orthodontics, surgery was done in which positive maxillomandibular relationship was achieved by mandibular setback using bilateral sagittal split osteotomy (BSSO) technique. (Fig: 7) The surgical phase will be followed by post-surgical orthodontics and retention phase will include Begg retainer and upper and lower bonded lingual retainers.
Treatment Alternative
The patient had no remaining growth due to which the best treatment option for the patient was a surgical approach.
Treatment results
Correction of skeletal discrepancies and dental problems allowed the occlusal, functional and aesthetic goals to be achieved. Class I canine relationships were established with proper alignment of the teeth. A positive overjet was established. Correction of malocclusion was accomplished with dental movement as well as with surgical repositioning of jaw.
Intraoral records demonstrated a satisfactory occlusal relationship in a lateral view, with good intercuspation and solid canine Class I relationship. From the frontal view, it was possible to observe the upper and lower dental midline coincidence and an adequate overbite. Because of the improvement in occlusion, the patient presented anatomical conditions to obtain satisfactory occlusal guides, with lateral movement guided by canine and protrusive movements by the incisors. (Fig: 8,9)
The patient did not show any TMD signs or symptoms after the surgery. Overall, she was satisfied with the improvement in her facial appearance and her normalized occlusal function.
Discussion
This case report describes the treatment of a female patient with dental and skeletal class III relationships. Surgical–orthodontic treatment was the best option for achieving an acceptable and stable occlusion as well as good esthetics in this case. An experienced multidisciplinary team approach ensures a satisfactory and stable outcome.
Presurgical orthodontics removes all the dental compensations and suggests the exact extent of the skeletal discrepancy. Normal skeletal base relationship is achieved by osteotomy and setback of the prognathic mandible (BSSO), postsurgical orthodontics guides the normal occlusal rehabilitation by correcting any emerging dental discrepancies.3
After thorough evaluation, the presurgical phase of orthodontic treatment was initiated with the aim to achieve ideal inter and intra-arch coordination, with each tooth in the correct position, with the goals of future surgical repositioning always being kept in mind.
The Angle Class III malocclusions can present a variable severity, with various levels of resolution complexity. Baccetti et al stated, the greater the skeletal involvement, the more complex the orthodontic treatment becomes. When the patient presents skeletal and dental disharmonies, usually with a significant facial impairment, a consequent psychosocial impact is expected. 4
Anne et al proposed, during the growth period, it is possible to establish orthopedic therapy to harmonize maxillomandibular growth. However, when the approach is too late, in post-pubertal stage with no growth potential, the options for treating these skeletal malocclusions become limited.5
Javed et al proposed that dental compensation can be planned without skeletal disharmony correction or a complete orthodontic therapy correction associated with orthognathic surgery.6,7
In the case described, the patient complained about, not only the dental aspect, but also the facial disharmony. For this reason, an orthodontic-surgical approach was proposed to correct skeletal discrepancy and to harmonize the face. After the treatment plan presentation and explanation by the surgeon regarding the surgical procedure, pre-surgical orthodontic treatment was started.
The result achieved by the surgery was very favorable, making easy the postsurgical phase and orthodontic finishing. The final treatment results were highly positive, achieved all the proposed objectives: significant improvement in facial profile and esthetics, in addition to functional and harmonic occlusion.
Postsurgical orthodontics is being done in this case for finishing and detailing of the occlusion and retention.
Conclusion
This case report shows that skeletal Class III with mandibular prognathism in a non-growing individual can be successfully managed using surgical–orthodontic treatment. Thus, careful case selection, patient cooperation and long-term stabilization ensures a successful treatment result.
Conflict of interest: None
Financial support and sponsorship: Nil
References
- Ellis III E, McNamara Jr JA. Components of adult Class III malocclusion. Journal of oral and maxillofacial surgery. 1984 May 1;42(5):295-305.
- Monson LA. Bilateral sagittal split osteotomy. InSeminars in plastic surgery 2013 Aug (Vol. 27, No. 03, pp. 145-148). Thieme Medical Publishers.
- Katiyar R, Singh GK, Mehrotra D, Singh A. Surgical–orthodontic treatment of a skeletal class III malocclusion. National journal of maxillofacial surgery. 2010 Jul;1(2):143.
- Baccetti T, McGill JS, Franchi L, McNamara JA Jr, Tollaro I. Skeletal effects of early treatment of Class III malocclusion with maxillary expansion and facemask therapy. Am J Orthod Dentofacial Orthop. 1998 Mar;113(3):333-43.
- Anne Mandall N, Cousley R, DiBiase A, Dyer F, Littlewood S, Mattick R, et al. Is early Class III protraction facemask treatment effective? A multicentre, randomized, controlled trial: 3-year follow-up. J Orthod. 2012 Sept;39(3):176-85.
- Javed O, Bernabé E. Oral Impacts on quality of life in adult patients with Class I, II and III malocclusion. Oral Health Prev Dent. 2016;14(1):27-32.
- Silvola AS, Varimo M, Tolvanen M, Rusanen J, Lahti S, Pirttiniemi P. Dental esthetics and quality of life in adults with severe malocclusion before and after treatment. Angle Orthod. 2014 July;84(4):594-9.

Figure 1: Pre-treatment extraoral photographs

Figure 2: Pre-treatment intraoral photographs
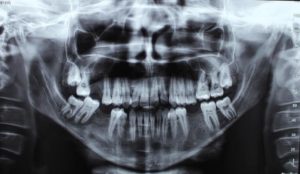
Figure 3: Pre-treatment OPG

Figure 4: Pre-treatment lateral cephalogram

Figure 5: Pre-treatment dental model

Figure 6: Presurgical phase – extraoral and intraoral photographs

Figure 7: During surgery; Mandibular setback using Bilateral Sagittal Split Osteotomy (BSSO) technique

Figure 8: Post-surgical phase extraoral photographs

Figure 9: Post-surgical phase – intraoral photographs

Figure 10: Post- surgical phase OPG

Figure 11: Post-surgical phase lateral cephalogram
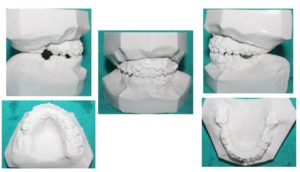
Figure 12: Post-surgical phase dental models

